By Vaidehi Gautam

Image from Scientific American
Preference of one gender over another, based on various forms of stereotypes, is known as gender bias. It can either be intentional or unconscious, and is subject to one’s social conditioning with respect to perception of different genders. Biological sex is different from gender. However, over a span of centuries, biological essentialism (i.e., the belief in sex-gender binary) has led to perpetuation of gender bias on grounds of biological differences between sexes. When it comes to medical sciences and healthcare, gender bias is a persistent issue even today. This bias results in faulty diagnosis as a result of which the patient suffers for a longer duration of time. Women are usually at the receiving end of this bias, both generally as well as in healthcare. This bias is usually manifested through inequality in the quality of treatment of women as compared to men for the same set of problems. Gender bias in healthcare is prevalent across a wide variety of health issues.
Bleeding Problems – Bleeding disorders such as haemophilia are conditions that restrict the clotting of blood in an effective manner. Both men and women may suffer from this problem. However, a study published in 2020 revealed that on average, women suffering from haemophilia get diagnosed 6.5 months later than men. There is no logical explanation for these delays. In fact, a large number of women are menstruators and it is more likely for them to notice bleeding problems due to their experience with monthly bleeding.
Mental Health – It is more likely for women to receive a diagnosis for a mental illness as compared to men. This bias is facilitated by the fact that women are subjected to gender-based violence and social inequity. However, such bias results in ignorance of the same symptoms among men who suffer with the same condition, and women end up being diagnosed with a disproportionately higher number of illnesses than they actually suffer from. Such bias affects both men and women.
Chronic Pain – despite being more prone to suffering from pains for a variety of natural reasons, women’s claims of severe pains are often dismissed due to the assumption that women are more sensitive and “hysterical”. In some cases, the pain is often diagnosed as something related to psychological issues in women as compared to men. This bias goes hand in hand with the above-mentioned bias pertaining to mental illnesses. Moreover, association of pain with menstruation often leads to lack of diagnosis of serious problems like endometriosis and cervical cancer in vagina-owners.
COVID-19 – Evidence suggests that the management of coronavirus pandemic could not remain untouched from gender bias. A 2020 analysis revealed that women who tested positive were less likely to receive X-rays and blood tests as compared to men who tested positive. Furthermore, the ongoing studies on the virus have failed to take gender and sex into account which has resulted in a gap in the research pertaining to how the virus is affected sexually different bodies and how much of these effects are being analysed on the basis of biased assumptions regarding genders.
The issue expands beyond these problems and the causes of such engendering of healthcare are rooted in sexism and systemic oppression of women in every field, even medical sciences. This sexism has manifested itself throughout history. It was not until the 20th century that women were even allowed to practice western medicine. A 2019 report from WHO suggests that despite significant representation of female doctors and researchers in medicine, the systemic sexism within the field still persists. Another root cause of this bias can be traced back to the practice of neglecting female bodies while conducting pioneering research regarding various illnesses. This neglect was the result of the assumption that male and female bodies differ only in terms of reproductive organs. Due to the lack of study of female anatomy, many problems related to women’s bodies are still a mystery today for healthcare professionals. This lack of knowledge is a result of persistent gender bias in the history of medical sciences.
The problem of gender bias in healthcare is being addressed and acknowledged in current scenarios. This is being done by recognising and analysing the main reasons behind the bias and the neglection of female bodies. More research is being conducted that involves women not only as the subject but also as the participants. Skewed participation is one big reason for gender bias, which is now being attempted for rectification. An approach towards educating the healthcare professionals of the bias is in place to help them understand the problem in a more nuanced manner. The problematic history of women’s problems in the healthcare realm have costed the lives of a disproportionately large number of women. An open conversation and increased participation of women is the key to address this problem and also provide an entry point for medical issues pertaining to the intersex and trans bodies.
Mary Poonen Lukose was an Indian gynecologist, obstetrician and the first female Surgeon General in India.[1] She was the founder of a Tuberculosis Sanatorium in Nagarcoil and the X-Ray and Radium Institute, Thiruvananthapuram, served as the head of the Health Department in the Princely State of Travancore and was the first woman legislator of the state.[1] The Government of India awarded her the fourth highest Indian civilian award of Padma Shri in 1975.[2]Mary Lukose, née Mary Poonen, was born to a rich family as the only child[3] on 2 August 1886[4] in Aymanam—a small village later made famous by being the setting of the novel The God of Small Things—[5] in the princely state of Travancore (modern day Kerala), in the British Indian Empire.[6] Her father, T. E. Poonen, was a medical doctor, the first medical graduate in Travancore and the Royal Physician of Travancore state.[1][4] Her mother had health issues due to which Mary was brought up by British governesses. She completed her schooling at Holy Angel's Convent High School, Thiruvananthapuram and topped the matriculation examination. However, she was denied admission for science subjects at the Maharajas College, Thiruvananthapuram (present day University College Thiruvananthapuram) for being a woman and had to pursue studies in history on which she graduated (BA) in 1909 as the only female student of the college and the first woman graduate of Madras University which Maharajas College was affiliated to.[1] As Indian universities did not offer admission to women for medicine, she moved to London and secured MBBS from the London University,[6] the first woman from what would later become Kerala to graduate in medicine.[7] She continued in the UK to obtain MRCOG (gynecology and obstetrics) from Rotunda Hospital, Dublin and underwent advanced training in pediatrics at the Great Ormond Street Hospital.[1] Later she worked in various hospitals in the UK and simultaneously pursued music studies to pass the London Music Examination.[1]
Mary returned to India in 1916, the year her father died,[3] took up the post of an obstetrician at the Women and Children Hospital, Thycaud in Thiruvananthapuram[7] and also worked as the superintendent of the hospital, replacing a westerner who had returned to her native place after marriage.[6] A year later, she married Kunnukuzhiyil Kurivilla Lukose (K. K. Lukose),[8] a lawyer who would later become a judge of the High Court of Travancore.[6] During her tenure at Thycaud Hospital, she initiated a midwifery training program for the children of local midwives in order to win over their support and is known to have delivered her first born at the hospital.[6] In 1922 she was nominated to the legislative assembly of Travancore,[9] known as Sree Chitra State Council, thus becoming the first woman legislator in the state.[6] Two years later, she was promoted as the Acting Surgeon General of the state of Travancore, making her the first woman to be appointed as the surgeon general in India.[6][10] She continued at the hospital till 1938 during which time she was nominated to the state assembly continuously till 1937.[6] In 1938, she became the Surgeon General, in charge of 32 government hospitals, 40 government dispensaries and 20 private institutions.[3] She is reported to have been the first woman to be appointed as the surgeon general in the world;[1][4][6][11] the first woman surgeon general in the US was appointed only in 1990.[3]
Mary was one of the founders of the Thiruvananthapuram chapter of the Young Women's Christian Association (YWCA) and became its founder president in 1918,[12] a position she retained till 1968.[6] She served as the Chief Commissioner of the Girl Guides in India[1][3] and was also a founder member of the Indian Medical Association and the Federation of Obstetric and Gynaecological Societies of India (FOGSI), which started as Obstetric and Gynaecological Society.[6] As the surgeon general of the state, she is reported to have founded the Tuberculosis Sanatorium in Nagarcoil, one of the first sanatoriums in India, which later grew to become the Kanyakumari Government Medical College.[13] She also founded the X-Ray and Radium Institute in Thiruvananthapuram.[6]
Mary and Lukose had two children, the eldest, Gracie, a medical doctor and a former assistant professor at Lady Hardinge Medical College, New Delhi[14] and the youngest, K. P. Lukose, former consul general, permanent representative of India to the United Nations and the Indian ambassador to Bulgaria.[6][4] Her husband died in 1947 and her two children also preceded her in death. She died on 2 October 1976 at the age of 90.[6] She was a recipient of the title, Vaidyasasthrakusala, from Chithira Thirunal Balarama Varma, the last Maharaja of Travancore.[1] The Government of India awarded her the civilian honour of Padma Shri in 1975.[2]
Source : https://en.wikipedia.org/wiki/Mary_Poonen_Lukose
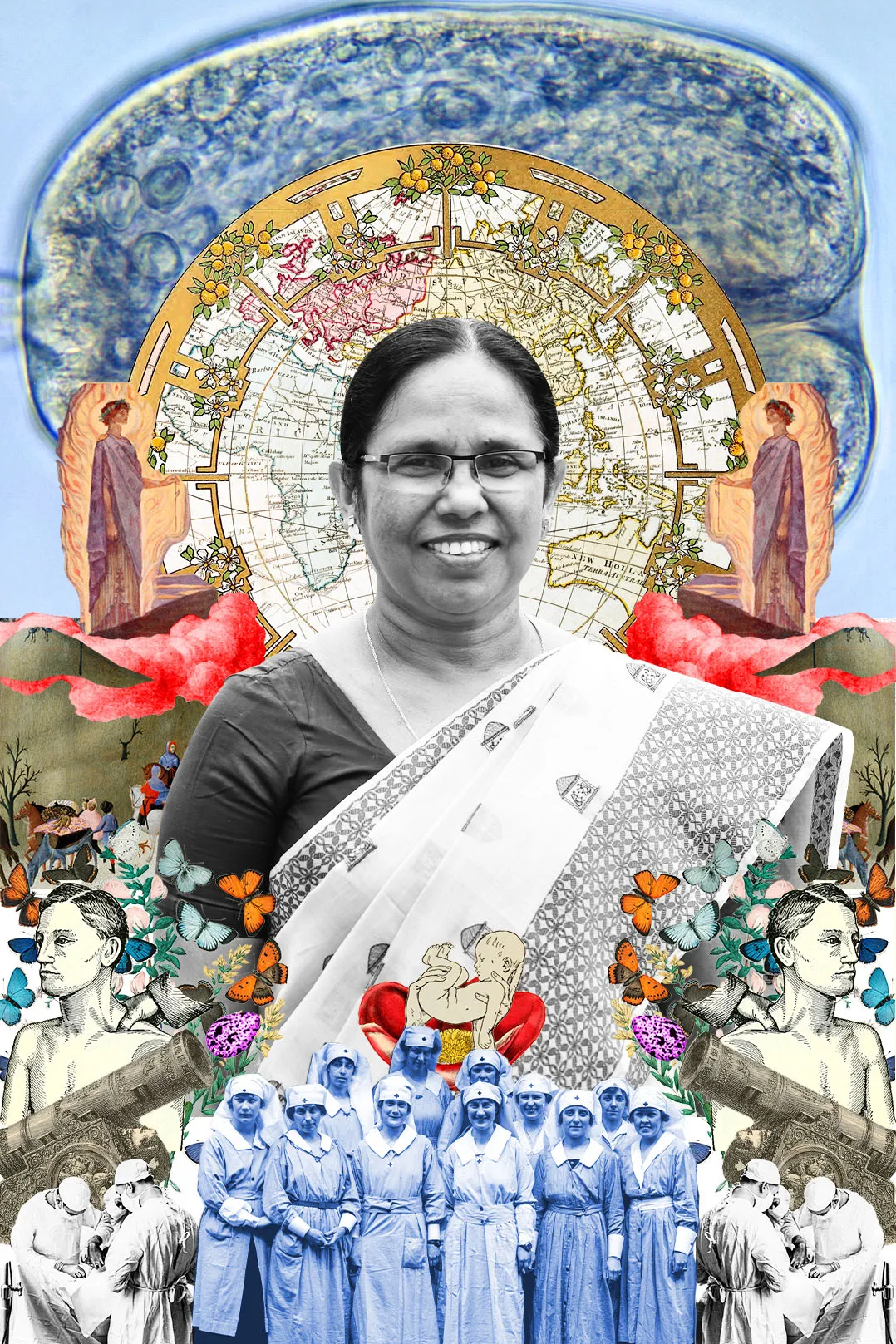
BY MANJU SARA RAJAN 7 MAY 2020
After the Nipah virus, KK Shailaja is now leading the way in the coronavirus battle with a focus on public healthcare.
It is lunchtime at the Secretariat in Thiruvananthapuram, Kerala’s capital city. The state Health, Social Justice and Woman and Child Development Minister KK Shailaja has taken out a bit of time for me from an exceptionally busy day during what is inarguably the most challenging period of her career. We are discussing the way her department has handled the coronavirus outbreak, and the reasons why Kerala appears to be better in control of it than many other places. Given her early career as an educator, the minister goes by the popular epithet Shailaja Teacher. The 63-year-old’s systematic approach and cohesive leadership together with Chief Minister Pinarayi Vijayan proved successful in managing the Nipah viral outbreak of 2018 and is once again, navigating Kerala through the current pandemic.
Flatten the curve
For weeks now there’s been talk about the ‘Kerala model’ of dealing with the Coronavirus pandemic, and how the state has managed to have India’s lowest mortality rate for this infection. On Sunday May 3, The News Minute reported that in an online media engagement Dr Raman Gangakhedkar, head of the Indian Council for Medical Research NIV, Pune, said, “Kerala is offering one of the best containment strategies and it is unparalleled. So we will continue to refer to the Kerala model as far as testing and containment strategies are concerned.”
So, how does a state with limited revenue end up being able to effectively manage a pandemic of such magnitude? Practice helps. Kerala has a long experience with infectious tropical diseases, like Chikungunya, H1N1, and more recently Nipah. Though the latter was then an unheard-of viral strain that jumped species to humans, the healthcare system was able to deal with the outbreak and contained its death toll to the districts where the outbreak began. “I think what worked for us was our systematic approach, communication with the public, and teamwork,” she says.
Back in action
As she was then, the health minister is back in the limelight now as commandant of the coronavirus battle. Shailaja Teacher says she read about the virus in China and knew they should prepare. “Wuhan University had students from Kerala, and we knew that if the students came back, we’d have to be careful. We formed a Rapid Response Team.”
On January 24, the government opened a control room to deal with the situation, made plans to isolate people, including home quarantine, and looked at the existing provisions of equipment including N95 masks, and PPEs (Personal Protective Equipment). On January 30, India registered its first Coronavirus infection in Kerala; it was a student who’d returned home from China.
As of May 4, 462 people have recovered from the infection in Kerala, and there have been just three deaths. Even the oldest patients have recovered—a couple, aged 88 and 93. “When their tests came back positive, they were moved to a medical college because they were very vulnerable,” she shares. “In fact, we had special nurses and the best ICU set aside for them. And so, we brought them back to life,” says Shailaja Teacher.
Public, private, primary
Kerala has long been focused on public health, education and social upliftment. Over the last few years, and since Shailaja Teacher got the health portfolio, there’s been renewed attention to the state’s public healthcare institutions. “We had a three-point agenda: government hospitals should be patient-friendly, high-tech, and out-of-pocket expenditure must reduce. Primary healthcare units are very important, especially in rural areas, they now have testing labs and are able to catch early signs of different diseases. Medical college hospitals have new equipment, and good infrastructure. Our focus definitely strengthened the system,” she says. After the experience with Nipah, the government implemented regular training for medical staff, who also underwent mock drills as preparation for an infectious outbreak.
Shailaja Teacher has often spoken of the healthcare system as a team. “We’ve tried to create a feeling of ‘We’,” she says. One of the ways in which they do that is a daily video conference with different frontline staff of the healthcare community across 14 districts. “Each day’s video conference is dedicated to groups of people doing different kinds of work, from district medical officers, nurses, ASHA workers. It gives us the opportunity to talk to people and hear them out. Keeping in touch with those working at the grassroots level is extremely important, we try to maintain that at all costs. When the minister, or a health secretary directly wants to understand their ground reality, it makes a huge difference, especially to keep morale up.” This style of functioning is also a reflection of Shailaja Teacher’s personal way of dealing with even a broad crisis. One of the students, who tested positive for COVID-19 after landing from China, has stated in interviews that the minister called her to reassure and wish her a speedy recovery.
Morale is especially important because there’s little knowing how things will pan out. Shailaja Teacher is cautious: “It will take time to get back to normal life. It is a truth that people must accept now. This virus is not like others. Many people test positive then test negative within a few days, but others take upward of 30 days to test negative. It sometimes takes five or six tests before it comes back negative. So that means this virus remains in the body for a while, and there’s a possibility of a transfer. In Kerala, we have it under control but if we get over-confident then we may have a second wave.”
Day to Day
When I spoke to Shailaja Teacher, she had another 9 or 10 hours of meetings, files, discussions, and even a press conference ahead of her. Her husband, two grown-up sons and their families, check in on her just before midnight via phone calls.
Her eldest lives in Dubai and recently became the second member of the family to deal directly with the pandemic. An electrical engineer, he was the project manager of a hospital construction project in Dubai. When the coronavirus infection broke out in the city, the government declared the hospital he was working on a COVID hospital. His team still works on the project and in case of maintenance and engineering works, he has to go into what is considered a high-risk environment. “I tell him to be careful and he tells me I should be careful. We keep warning one another,” she says.
Vogue Warriors shines the spotlight on the women at the medical frontlines and essential services—doctors, nurses, scientists, innovators—alongside behind-the-scene heroes working tirelessly to help us through the ongoing pandemic.
Source : https://www.vogue.in/culture-and-living/content/vogue-warriors-kk-shailaja-kerala-health-minister-covid-19-response